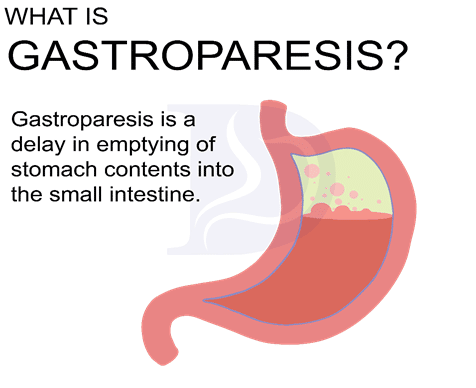
Gastroparesis is delayed stomach emptying due to altered gastric motility.1 Usually, the stomach contracts three times per minute. Strong muscular contractions of the stomach help digest food and push it towards the small intestine.
In gastroparesis, stomach motility is reduced and digestion and gastric emptying are delayed. Symptoms of gastroparesis can overlap with those of acid reflux so you should see a physician to determine the severity of your case.
Causes of Gastroparesis
The exact reason for gastroparesis is still being studied. In nearly 36% of gastroparesis cases, the causes are unknown. Most cases are due to one or more of the following:
Nerve damage
Studies have linked gastroparesis with disrupted nerve signals. The vagus nerve controls digestion and stomach contractions. When nerve damage occurs, stomach contractions and movement are slowed resulting in delayed emptying.
Post-surgical
Approximately 13% of gastroparesis cases are believed to be associated with surgical procedures.
Diabetes
Elevated glucose levels in the blood lead to nerve signaling disruption, which ultimately affects digestion. Diabetes affects the vagus nerve, which controls digestion and gastric motility.
Medications
Some drugs like L-dopa, hyoscyamine, Bentyl, Levsin, and narcotics can weaken the stomach.2
Mental Disorders
Parkinson's disease, stroke, and brain injury can lead to altered digestive function.
Scars and fibrous tissue
Scars from tumors and ulcers can block the lower esophageal sphincter, mimicking gastroparesis.
Symptoms
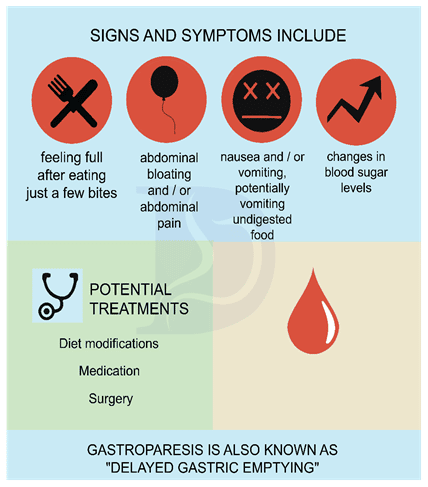
The following symptoms are commonly observed3:
- Feelings of gastric fullness even after taking just a few bites of food
- Bloating, excessive belching, and nausea after eating
- Vague, mild pain in the upper abdomen
- Heartburn, vomiting, and backflow of stomach contents into the mouth
- Lack of appetite
- Changes in blood sugar levels
- Weight loss due to undernourishment
Diagnosis
First, a detailed history will be obtained by your provider.
X-ray
An upper GI barium X-ray can help monitor when liquid barium leaves the stomach. A delay in emptying would indicate gastroparesis.
Endoscopy
The stomach is examined for visual abnormalities such as inflammation, ulcers, residual food, and bleeding.
Gastric Emptying Test
This is a confirmatory test for the diagnosis of gastroparesis. In this test, food like scrambled eggs will be labeled with markers that can be seen from a scanner. The scanner notes the time it takes for the food to leave the stomach.4 After 4 hours, less than 10% of the stomach contents should be present in a normal sample.
Electrogastrogram (EGG)
This test is used to measure electrical waves produced by the stomach.5
Treatment
The first step in treatment is control of underlying causes of gastroparesis such as diabetes. Medications may also need to be adjusted as necessary.
Dietary changes
- Liquid diets and shakes are recommended because they travel through the stomach more quickly than solid foods.
- Smaller meals eaten 5–6 times per day are recommended as opposed to the traditional 3 large meals per day.
- Diets high in fiber should be limited, as they delay gastric emptying.
Medications
Different medications are available that will stimulate the stomach and increase contractions. Metoclopramide, Domperidone, Bethanechol, and Bo-Tox are commonly used in the treatment of gastroparesis.
Electrical stimulation
High-frequency electrical neurostimulation of the stomach at 12 cycles/minute can be helpful in increasing gastric motility. Gastric pacing aims to provide energy for contractions.6
G-POEM (gastro per-oral endoscopic pyloromyotomy)
This procedure involves cutting the pylorus. G-POEM is considered a last resort option for patients who have tried all other remedies without success.
Summary
Gastroparesis is a medical condition caused by slow emptying of the stomach after eating. Once diagnosed, the best approach to management is usually dietary modifications and lifestyle changes to ease symptoms.
References
- Camilleri M, Chedid V, Ford AC, et al. Gastroparesis. Nat Rev Dis Prim. 2018;4(1). doi:10.1038/S41572-018-0038-Z
- Liu N, Abell T. Gastroparesis Updates on Pathogenesis and Management. Gut Liver. 2017;11(5):579. doi:10.5009/GNL16336
- Reddivari AKR, Mehta P. Gastroparesis. StatPearls. Published online December 31, 2021. Accessed May 18, 2022. https://www.ncbi.nlm.nih.gov/books/NBK551528/
- Friedenberg FK, Parkman HP. Delayed gastric emptying: whom to test, how to test, and what to do. Curr Treat Options Gastroenterol. 2006;9(4):295-304. doi:10.1007/S11938-006-0011-X
- Calder S, O’Grady G, Cheng LK, Du P. A Theoretical Analysis of Electrogastrography (EGG) Signatures Associated With Gastric Dysrhythmias. IEEE Trans Biomed Eng. 2017;64(7):1592-1601. doi:10.1109/TBME.2016.2614277
- Stein B, Everhart KK, Lacy BE. Gastroparesis: A Review of Current Diagnosis and Treatment Options. J Clin Gastroenterol. 2015;49(7):550-558. doi:10.1097/MCG.0000000000000320