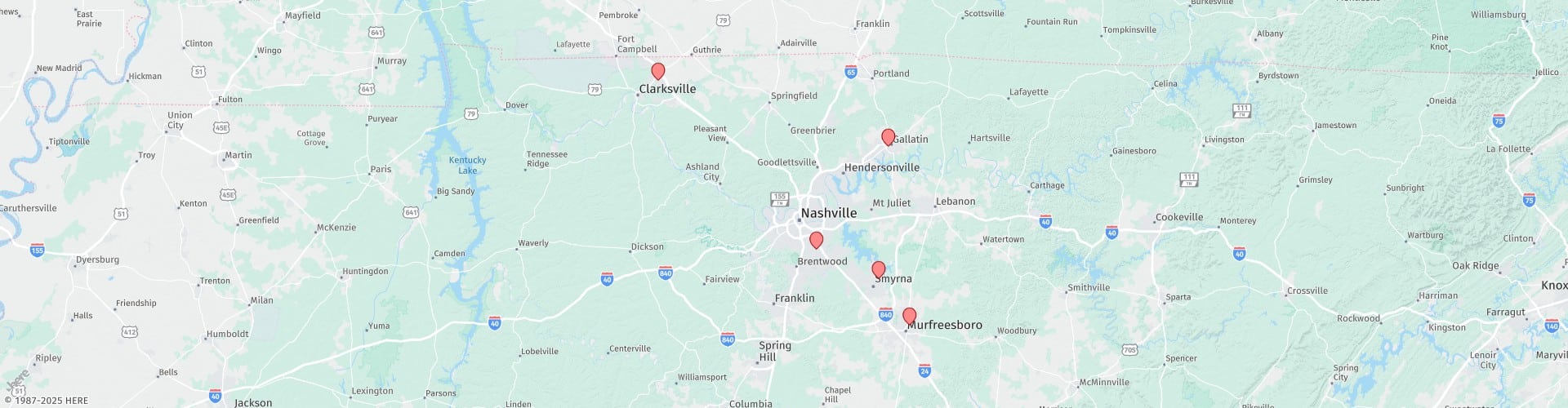
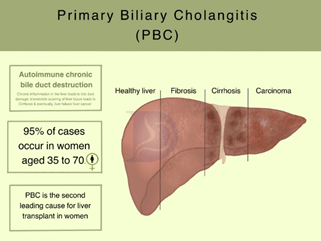
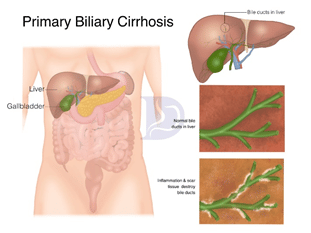
Primary biliary cholangitis, formerly called primary biliary cirrhosis, is any damage to the bile ducts in the liver.1 Bile ducts are small channels carrying bile from the liver to the small intestine. In the intestine, the bile helps digest fats through emulsification. Bile also helps absorb fat-soluble vitamins like A, D, E, and K.
If the bile ducts are damaged, it leads to a build-up of bile in the liver, which can damage the liver and lead to cirrhosis. In chronic cases, the liver becomes inflamed, scarring of bile ducts occurs, and the ducts are destroyed permanently.
Causes
The exact cause of PBC is still unknown, but research shows that there is typically more than one contributing factor for this disease. The major cause of the disease is an autoimmune reaction, a condition in which the body considers the organs as foreign material and fights against them.2
Stages of PBC
Based on the severity, PBC has four stages:
Stage 1: Medium-sized bile ducts are inflamed and damaged.
Stage 2: Small-sized bile ducts are blocked in this stage.
Stage 3: When the scarring of the liver starts, it is referred to as stage 3.
Stage 4: Permanent, severe scarring and cirrhosis has developed in the liver.
Symptoms
Initially, the symptoms of PBC are not prominent. Only a blood test can show elevated alkaline phosphatase levels in the early stages. Fatigue and itching may occur as the bile enters the bloodstream. The following symptoms are common:
- Belly pain
- Darkening of skin
- Loss of appetite
- Nausea
- Weight loss
- Yellow bumps under skin and eyes
- Muscle, joint, and bone pain
- Swollen belly with fluid build-up
- Weakened bones and fractures
- Diarrhea
- Immune-related problems
- Thyroid and arthritis problems3
Diagnosis
Different tools are used to diagnose PBC at the different stages. Initially, fatigue and itching may indicate a possibility of PBC. A high level of liver enzymes also helps in diagnosis at an early stage.4
Mitochondria antibody test
This is an important diagnostic test for PBC. Mitochondria antibodies are produced in the body in 95% of cases. A physician can ask questions to determine other relevant symptoms along with checking for elevated mitochondria antibodies.
Ultrasound
A physician might ask for an ultrasound of the gall bladder, bile ducts, and liver. Ultrasound scanning will help the doctor see bile duct obstructions. Other images like CT scans and MRIs can also be taken to get more information.
Liver biopsy
In chronic cases, a liver tissue sample is taken to check how much damage has occurred to the liver. To take the sample, a small needle is inserted through the lower chest under local anesthesia.
Treatment
Treatment aims to reduce symptoms as the disease progresses. Questran is an effective drug that not only treats itching but also binds with bile and does not allow it to be reabsorbed into the bloodstream.
Diet
PBC can weaken the bones and lead to osteoporosis. A daily dose of 1200 mg of calcium is recommended with PBC. Vitamin D intake should also be increased because it helps with calcium absorption in the intestine.
Drugs
The following drugs are effective against PBC:
- Ursodeoxycholic acid (Actigall) effectively changes the bile make-up in the liver and protects the liver from bile damage.5
- Colchicine helps reduce itching associated with PBC.
- Obeticholic acid (Ocaliva) targets the proteins involved in bile acid production.
If no improvement occurs, a liver transplant is the last resort.
References
- Pandit S, Samant H. Primary Biliary Cholangitis. StatPearls. Published online May 8, 2022. Accessed August 9, 2022. https://www.ncbi.nlm.nih.gov/books/NBK459209/
- Purohit T, Cappell MS. Primary biliary cirrhosis: Pathophysiology, clinical presentation and therapy. World J Hepatol. 2015;7(7):926. doi:10.4254/WJH.V7.I7.926
- Khanna A, Leighton J, Lee Wong L, Jones DE. Symptoms of PBC - Pathophysiology and management. Best Pract Res Clin Gastroenterol. 2018;34-35:41-47. doi:10.1016/J.BPG.2018.06.007
- Hirschfield GM. Primary Biliary Cholangitis: Clinical Insights Into Diagnosis and Staging. Gastroenterol Hepatol (N Y). 2021;17(5 Suppl 5):2. Accessed August 9, 2022. /pmc/articles/PMC8191838/
- Heathcote J. Treatment of primary biliary cirrhosis. J Gastroenterol Hepatol. 1996;11(7):605-609. doi:10.1111/J.1440-1746.1996.TB00300.X