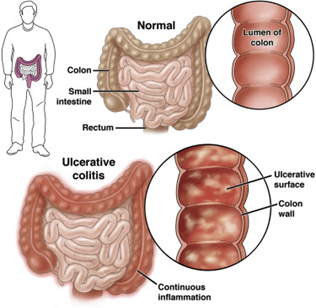
Inflammatory bowel disease is a chronic infection of the gastrointestinal tract. This wide term is used for a group of intestinal diseases that causes inflammation of the intestine. It has two types:
- Crohn’s Disease
- Ulcerative Colitis1
There is not much difference between these two, but if we observe keenly, we know that Crohn's disease causes inflammation of any part of the digestive tract, the small intestine mostly, while Ulcerative Colitis causes inflammation of the rectum, part of the large intestine.
Symptoms of IBD
IBD has several signs and symptoms that must be recognized early, and some of the most important symptoms are2:
- Diarrhea
- Constipation
- Fatigue
- Abdominal pain, cramping and bloating
- Rectal bleeding
- Weight loss and anaemia
- Decreased appetite
- Children with IBD may have decreased growth and development
Symptoms of IBD outside of the GI tract:
- Skin disease
- Joint pain and osteoporosis
- Eye infection
Causes of IBD
The definitive cause of IBD is unknown, but the factors that can lead to IBD are3:
- Genetic factors and family history play a vital role.
- Weak immune system. If your immunity is weak, then you are more susceptible to several diseases, especially IBD.
- Smoking is one of the main risk factors for getting Crohn's disease.
- It is present in all populations, but according to various studies and research, it is said that IBD is more common among white people.
- It is observed that people older than age 35 are more vulnerable to this disease.
- Environmental factors are also responsible for having IBD, such as IBD is more common among people living in northern climates, where the weather is mostly cold.
- IBD has the same effect on males and females, but it is seen that Ulcerative Colitis is more common among men older than 45 years, while Crohn's disease is more prevalent among girls over the age of 14.
- Long-term use of non-steroidal anti-inflammatory medicines such as ibuprofen, naproxen sodium (Aleve), and diclofenac sodium have adverse effects on GI tract.
Complications
- Malnutrition
- Colorectal cancer
- Fistulas
- Bowel obstruction
- Blood clots
Diagnosis
History is very important in diagnosing IBD, followed by one or more physical tests4:
Barium enema
X-ray to examine the colon and small intestine.
Flexible sigmoidoscopy and colonoscopy
Uses a camera to look inside the GIT for fistulas, ulcers, and other abnormalities. Colonoscopy is used to examine the entire length of the large intestine.
Capsule endoscopy
Mostly used to inspect the small intestine. You have to swallow a capsule containing a camera that shows an inner picture of the GIT.
Plain X-ray
Used in emergency cases to rule out intestinal ruptures.
CT and MRI Scans
CT and MRI studies are quite helpful in diagnosing inflammation or other complications of disease such as fistulas and abscesses.
Treatments
There are certain treatment options available for IBD.
Medications
Anti-inflammatory drugs such as:
- Corticosteroids in the form of prednisone, methylprednisone.
- Aminosalicylates and 5ASA drugs such as balsalazide are used to reduce inflammation, particularly in the small intestine and colon.
- Immunomodulators (methotrexate, azathioprine) prevent the immune system from attacking the GIT.
- Biologics work by inhibiting the TNF factor, an inflammatory chemical produced by the immune system.
- Antibiotics for killing bacteria.
- Antidiarrheal medications and laxatives for relieving diarrhea and constipation.
Lifestyle changes
Drink an adequate amount of water to cope with diarrhea, and avoid stress because it also triggers inflammatory responses. Quit smoking. Avoid eating spicy foods.
Supplements
Iron supplements help in treating anaemia.
Surgery
Surgery is an option if medication therapy is not helping to maintain symptoms and flares.
- Strictureplasty
- Removal of fistulas
Removal of affected parts of the GI tract
References
- McDowell C, Farooq U, Haseeb M. Inflammatory Bowel Disease. StatPearls. Published online May 1, 2022. Accessed June 10, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470312/
- Perler B, Ungaro R, Baird G, et al. Presenting symptoms in inflammatory bowel disease: descriptive analysis of a community-based inception cohort. BMC Gastroenterol. 2019;19(1). doi:10.1186/S12876-019-0963-7
- Rubin DC, Shaker A, Levin MS. Chronic intestinal inflammation: inflammatory bowel disease and colitis-associated colon cancer. Front Immunol. 2012;3(MAY):107. doi:10.3389/fimmu.2012.00107
- Seyedian SS, Nokhostin F, Malamir MD. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J Med Life. 2019;12(2):113. doi:10.25122/JML-2018-0075